Content
- general information
- ICD-10 disease code
- Pathogenesis of tuberculosis of lymph nodes
- Classification and forms
- Morbidity risk group
- Possibility of infection
- What is the difference from oncology
- Symptoms of tuberculosis of the lymph nodes
- Common signs
- Peripheral lymph nodes
- Intrathoracic lymph nodes
- Tuberculous mesenteric adenitis
- Stages and features of the course of the disease
- In adults
- In children
- Identification of tuberculosis of the lymph nodes
- Who is engaged in diagnostics
- Diagnostic methods
- How is tuberculosis of the lymph nodes treated?
- Chemotherapy (early stage)
- Surgical intervention
- Cleaning and rinsing
- Physiotherapy measures
- ethnoscience
- Complications of lymph node tuberculosis
- Rehabilitation period
- Recovery prognosis
- Disease prevention
Lymph node tuberculosis is a common extrapulmonary form of the disease. It affects mainly young women, less often men under 25 years of age. In children, pathology is less common, but their pathology often proceeds with severe complications. This disease requires timely diagnosis and complex treatment, because in case of late detection, surgical intervention is necessary to improve the patient's condition.

general information
Lymph nodes are essential for immune function. They form specific antibodies that fight pathogenic microorganisms. If the lymphatic system is immature or there is a sharp deterioration in the work of defense mechanisms, mycobacteria enter the nodes, leading to the development of an inflammatory-allergic reaction.
Mass vaccination and the use of antibiotics have led to the fact that tuberculous lymphadenopathy is more often primary in nature, i.e. the inflammatory focus is formed immediately in the nodes. However, a secondary one is also possible, in which the infection spreads through the vessels from the lungs or other organs.
Relatively rarely, intrathoracic lymph nodes (IHLN) are affected, more often peripheral ones are affected.
In most cases, the disease progresses slowly and is chronic. Pronounced symptoms occur only during a period of a strong decrease in immunity, when mycobacteria begin to multiply rapidly in a nutrient medium. After an exacerbation, remission can spontaneously occur, but if the protective mechanisms do not work, life-threatening complications develop.
ICD-10 disease code
According to the international classification of diseases, tuberculosis of the lymph nodes, confirmed by histological or bacteriological studies, marked with code A15.4. If specific tests were not performed and the diagnosis was made on the basis of the clinical picture, the pathology is indicated as A16.3.

Pathogenesis of tuberculosis of lymph nodes
Macrophages of the stroma of lymphoid tissue are able to absorb mycobacteria, placing them in their cytoplasm. Subsequently, phagolysosomes are formed. However, mycobacteria have a dense membrane that protects them from enzymes. Bacilli do not die, but they do not reproduce either. During this period, latent tuberculosis can be diagnosed.
Mycobacteria, upon the onset of favorable conditions for them, quickly spread through the lymphatic system, affecting 1 or a group of intrathoracic or peripheral lymph nodes. Koch's wand begins to multiply rapidly, provoking a local allergic reaction and inflammation. Tissues react sharply to infection.
The immune system is activated. Cytokines and monocytes are involved in the formation of special phagocytic granulomas from macrophages transformed by the action of mycobacteria. In the tissues of the lymph nodes, metabolic processes are disrupted. In most cases, this leads to the formation of foci of caseous necrosis.
In the future, spontaneous healing may occur. Relapse often occurs with the activation of the L-forms of Koch's bacillus.
Classification and forms
Depending on the location of the damaged elements, there are 3 types of the disease:
- abdominal mesenteric adenitis;
- tuberculosis of the cervical nodes;
- bronchoadenitis.

The most rare is abdominal mesenteric adenitis. It is characterized by the defeat of the retroperitoneal and mesenteric nodes. In most cases, this form of the disease is secondary, i.e. mycobacteria enter the lymphatic system from a primary focus located in the intestine or stomach.
Tuberculosis of the cervical lymph nodes is also relatively rare. More often, the disease is of a primary nature, i.e. mycobacteria flow from the external environment. Mostly paratracheal or submandibular nodes are affected.
Bronchoadenitis is the most common form of extrapulmonary tuberculosis. It is characterized by damage to the basal, bronchopulmonary nodes, as well as elements of the lymphatic system located in the mediastinal region.
Important information: How does eye tuberculosis manifest?
There are 3 options for its course:
- Focal. It is more often diagnosed in newborns and is accompanied by a strong increase in lymph nodes (up to 5 cm in diameter). Overgrowth of tissues and the formation of caseous necrosis inside the capsule are observed. Soldering of nodes and the formation of conglomerates often occur. This complicates the therapy of the disease.
- Infiltrative. In this case, the lymph nodes increase slightly. Perinodular inflammation is detected, which can go beyond the capsule. Infiltration of the basal parts of the lungs is often detected.
- Small. There is a slight increase in lymph nodes. However, they are firm and well palpable. 1-2 elements are affected. At the same time, symptomatic manifestations are poorly expressed.
The violation can be both primary and secondary. However, mycobacteria often enter the nodes from the focus located in the lungs.
Morbidity risk group
Tuberculous lesion of the lymphatic system develops after the penetration of mycobacteria into the human body. Infection often occurs by airborne droplets and contact.

A special risk group for the development of pathology includes people living in unfavorable conditions, including:
- patients of drug treatment clinics;
- residents of nursing homes;
- refugees;
- migrants;
- homeless, etc.
Intrauterine transmission of mycobacteria from mother to child is also possible. The first signs of the disease appear only after the end of the incubation period, which can last from 4 to 8 months. In addition, there are a number of factors that contribute to the activation of mycobacteria in the human body.
These include:
- diabetes;
- HIV infection;
- the use of certain medications;
- avitaminosis;
- undergoing immunosuppressive therapy;
- long experience of smoking;
- alcoholism;
- nutritional deficiencies, etc.

The risk of developing tuberculosis is increased in people who have not received the BCG vaccine and do not have immunity to mycobacteria.
Possibility of infection
Mycobacteria are resistant to the influence of environmental factors and can persist for a long time on different surfaces. However, if the immune system is working normally, it detects mycobacteria in a timely manner and destroys them.
With regular ingestion of Koch's bacillus into the body against the background of weakening of the protective mechanisms, infection occurs. A sick person is contagious only if the pathology progresses and its transition to an open form, in which mycobacteria begin to be released into the environment.
What is the difference from oncology
Tuberculosis, unlike oncology, is an infectious disease. The pathogen can be transmitted from person to person. People with malignant tumors cannot infect others. At the same time, both with oncology and with tuberculosis, lymph nodes can increase and other symptoms that are similar for both disorders appear.
Symptoms of tuberculosis of the lymph nodes
The clinical picture of the disease consists of general manifestations and specific signs of damage to certain nodes.
Common signs
With the defeat of the lymphatic system by mycobacteria in patients, an increase in the manifestations of general intoxication is observed.

These include:
- nausea;
- weakness;
- increased body temperature;
- increased sweating;
- loss of appetite;
- weight loss;
- diarrhea;
- stomach ache;
- anemia;
- tachycardia;
- fast fatigability, etc.
Peripheral lymph nodes
Tuberculosis of peripheral lymph nodes is accompanied by tissue edema. The elements grow up to 1-3 cm in diameter. Compaction of the affected tissues occurs. In addition, the nodes located in the neck and armpits are well palpable. They are painful and mobile to the touch.
Intrathoracic lymph nodes
Tuberculosis of the intrathoracic lymph nodes in children and adults is accompanied by chest pain, severe sweating, fever and cough. Often there is an expansion of the venous network located on the front of the chest.

Tuberculous mesenteric adenitis
Tuberculosis of the mesenteric lymph nodes is accompanied by severe bloating, vomiting, indigestion, stool disorders, pain, etc.
In the acute course of the disease, the symptoms are similar to those of gastroenteritis or appendicitis.
Stages and features of the course of the disease
There are 4 stages of the pathological process:
- First. It is characterized by primary infection and the formation of granulomatous foci. During this period, there are no characteristic symptoms of tissue damage.
- Second. Infection intensifies and granulomas grow rapidly. In the center of the formations, necrosis is formed. The death of tissues leads to the appearance of characteristic signs of intoxication.
- Third. The affected area begins to soften. The pathological process turns into a purulent form. The development of a "cold" abscess is observed.
- Fourth. Several large granulomas are formed, which are located close to the skin. There is a risk of the formation of cartilaginous passages. Often, purulent masses melt the surrounding tissue and come out.
Important information: What is primary tuberculosis complex
In adults
In such people, damage to the lymphatic system occurs due to the spread of mycobacteria through the vessels from the primary focus, localized in the lungs. Often, the course of the disease is complicated by the formation of a bronchopulmonary fistula, which causes a severe cough. Basal fibrosis often develops. In adults, large areas are formed, inside which there is a curdled necrotic mass.

The defeat of the lymph nodes in adults in most cases is observed due to the progression of immunodeficiency against the background of HIV infection.
In children
They are more likely to have lesions of peripheral nodes. The first and second stages can be asymptomatic. The exception is when the child has an increased sensitivity to infection. This leads to an increase in temperature and the appearance of signs of an inflammatory process. The nodes become hard and painful. The skin above them turns red. Complications appear.
Identification of tuberculosis of the lymph nodes
Tuberculous lesion of the lymph nodes requires a comprehensive diagnosis. When signs of a disease appear, you need to contact a specialist who will prescribe the necessary studies.
Who is engaged in diagnostics
The diagnosis is carried out by a phthisiatrician, but if necessary, narrowly focused specialists can be involved.
Diagnostic methods
First of all, the doctor conducts a physical examination and analyzes the patient's complaints.

After that, immunological tests are prescribed:
- Mantoux.
- Diaskintest.
- Quantiferon test.
To identify foci in the lungs that differ in a more typical localization, radiography and endoscopy of the bronchi are prescribed. Additionally, ultrasound of the abdominal organs and CT of the thoracic region are required. In addition, patients are prescribed general and biochemical blood tests. A biopsy is often done to confirm the diagnosis. The selected materials are then sent for histological examination.
How is tuberculosis of the lymph nodes treated?
If the disease is detected at an early stage, therapy can be carried out with a combination of medications. It is permissible to use folk recipes and physiotherapeutic measures. In more advanced cases, surgery is required.
Chemotherapy (early stage)
For chemotherapy, 2-4 antibiotics are most often prescribed, which are active against mycobacteria. These drugs include Isoniazid, Ethambutol, Rifampicin, and Pyrazinamide. The course of treatment is 9 to 12 months.
Additionally, patients are recommended to take vitamins. Drugs designed to suppress the activity of mycobacteria are highly toxic, so patients are prescribed hepatoprotectors.
These funds include:
- Hepabenne.
- Carsil.
- Phosphogliv.
- Essentiale.
Additionally, funds are selected to eliminate symptoms.
To suppress inflammation and eliminate fever, nonsteroidal anti-inflammatory drugs (NSAIDs) are prescribed:
- Ibuprofen.
- Nimesulide.
- Nurofen, etc.

Complex therapy helps to eliminate clinical manifestations and destroy mycobacteria.
Surgical intervention
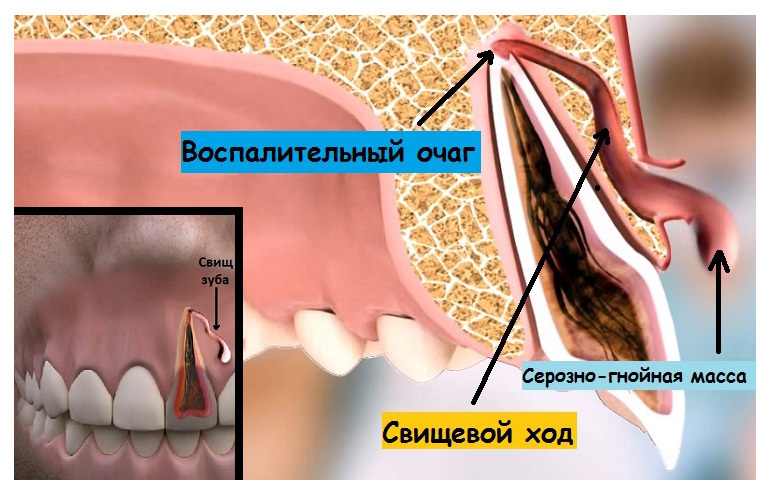
When necrosis foci are formed in the nodes, in most cases, surgical intervention cannot be avoided. In addition, the indication for the operation is the ineffectiveness of conservative treatment within 3-4 months.
During the intervention, the elimination of the formed granuloma and suturing of the fistulous passages are performed (if necessary). In severe cases, the damaged lymph nodes are removed.
Cleaning and rinsing
The node cleaning operation is performed under general anesthesia. The site of inflammation is accessed through a small incision. After that, the contents of the damaged area are drained. The cavity is washed with sterile saline and then with a disinfectant solution. After that, it is sutured for healing.

Physiotherapy measures
Patients with tuberculous lesions of the lymph nodes are recommended to be treated in a sanitary environment.
Important information: What you need to know when donating blood for tuberculosis
Great benefits are brought by:
- electrophoresis;
- Exercise therapy;
- breathing exercises;
- medicinal baths;
- mud therapy, etc.
These procedures help to activate the immune system and suppress the activity of mycobacteria faster.
ethnoscience
There are many traditional medicines that can be used to treat tuberculous lesions of the lymph nodes. The use of dried bear is recommended. The insect must be crushed into powder and eaten with plenty of water.

Some healers recommend taking a series of baths.
To prepare a healing agent you need:
- Pour 5 liters of boiling water over 1 kg of grass and leave for 15 minutes.
- Strain the infusion and pour into the bath.
To strengthen the immune system, it is recommended to consume medicinal tea.
To prepare it you will need:
- Grind 100 g of currant leaves, 75 g of calendula and the same amount of budra.
- Mix all components thoroughly.
- Pour 1 tbsp. mixture of 150 ml of water.
- Drink the product 4 times a day.

A positive effect can also be achieved when using compresses based on a decoction of ginger root.
To prepare the product you need:
- Extract about 25 g of the root and boil it in 100 ml of water for 15 minutes.
- Strain the liquid and use it to apply compresses.
- Apply them for at least 3 hours.
Complications of lymph node tuberculosis
Most often, the defeat of the lymph nodes leads to the development of such a dangerous complication as a breakthrough of the caseous focus of necrosis. If the nodes are located in the abdominal cavity, it will lead to the development of severe peritonitis. If nodes in the neck and armpits are affected, there is a high risk of the contents being released.
In addition, possible complications include:
- segmental atelectasis of the lung;
- fistulous passages;
- catarrhal endobronchitis;
- broncholithiasis;
- pulmonary bleeding;
- exudative pleurisy, etc.
In addition, in rare cases, against the background of damage to the cervical nodes, mesenteric thrombosis occurs. This is an extremely dangerous condition that is often fatal. The complication occurs more often in adults.
Rehabilitation period
During this period, patients need to avoid physical and emotional overload, regularly walk in the fresh air. In addition, it is advisable for them to go to physiotherapy, exercise exercise therapy, adhere to a sparing diet and all the doctor's recommendations. The rehabilitation period takes 3-6 months.
Recovery prognosis
With timely detection and the beginning of complex therapy, the prognosis for recovery is favorable. If the disease proceeded with complications, it is highly likely that the disease will become chronic and will be accompanied by pronounced periods of exacerbations and remissions. In rare cases, this type of extrapulmonary tuberculosis is fatal.
Disease prevention
Vaccination is an effective method of drug prevention of tuberculosis. BCG vaccinations are performed for children in the hospital in the first days of life. This reduces the risk of infection in the child in the future. Re-vaccination is done at 7-8 years old. Adults are advised to undergo fluorography every six months.
In addition to drug prevention methods, there are additional methods that can significantly reduce the risk of tuberculosis:
- compliance with the rules of personal hygiene;
- washing hands after using public transport;
- hardening;
- frequent walks in the fresh air;
- regular sports;
- proper nutrition;
- rejection of bad habits;
- timely treatment of infectious diseases, etc.
In addition, it is recommended to undergo regular examinations and timely conduct therapy for exacerbations of all existing chronic diseases. For people who often suffer from vitamin deficiency, it is advisable to regularly take multivitamin complexes. The use of techniques that enhance immunity can reduce the risk of infection with mycobacteria.
People who exercise regularly have a healthy diet and do not have chronic infectious diseases, infection with tuberculosis extremely rarely turns into a generalized form, which is dangerous for life.



